Falls are one of the most insidious threats to healthcare facilities, especially in long-term care. Mindful facility administrators and clinical directors put fall prevention programs in place to ensure their residents and staff are as safe as possible. But what are the best strategies for preventing falls in long-term care? Read our tips from a certified fall prevention specialist to augment the protections you have in place.
Key Facts About Falls
These facts should serve as a call to action to all healthcare facilities to invest in fall prevention programs that work. Both clinical and community-based solutions have been shown to be effective at reducing the frequency of falls in long-term care facilities and beyond. The first step in preventing falls is to recognize what causes them in the first place.
Top 5 Fall Prevention Strategies
Falls don’t have to be a normal part of aging. There are many ways that healthcare professionals and families can protect their loved ones from the risk of injury.
- Monitor Overall Health – Check in with your residents on a regular basis to determine their individual fall risk. Make any necessary changes to their treatment plan.
- Environment & Facility Design – Choose flooring, furniture, and storage options that provide optimal safety and always ensure cleanliness throughout the facility.
- Ensure Proper Clothing & Footwear – Make sure footwear supports the foot and provides a stable standing surface. Choose shoes with grippy, non-slip soles.
- Evaluate Personal Needs Frequently – Does the resident feel the urge to attend to a personal need (i.e., use the restroom, get a drink)? Nursing staff should frequently evaluate these needs and provide prompt assistance.
- Choose the Right Equipment – Wheelchairs, canes, walkers, and rollators can all help or hurt an individual’s fall risk. Make sure the equipment is well suited to the resident’s needs. Avoid one-size-fits-all solutions.
Let’s take a deeper look at each of these strategies.

Who is At-Risk for a Fall?
There are many factors that play into an individual’s risk of injury due to a fall. It’s important to consider the full picture in order to identify those risks and reduce them as much as possible.
Common Causes of Falls Include:2
- Muscle weakness
- Environmental hazards
- Certain medications
- Poor footwear and foot care
- Vitamin D deficiency
- Low vision or depth perception problems
- Uneven flooring surfaces
- A diagnosis that causes instability or balance issues
An In-Depth Look at the Risk Factors
Most falls are due to a combination of risk factors. A fall history in the last six months is the most predictive factor of a future fall, along with intrinsic factors, including comorbidities. This is especially true if an individual is diagnosed with dementia, hip fracture, diabetes, Parkinson’s disease, or arthritis. Issues with cognitive function, balance, gait, or vision can also contribute to a higher fall risk. External factors can play a role as well, such as inappropriate footwear, uneven flooring surfaces, clutter, and malfunctioning medical equipment (i.e., canes, walkers, and wheelchairs).
How to Design a Long-Term Care Facility to Reduce Falls
The environment in a skilled nursing facility can play a large role in fall prevention. From the furniture you select to the tidiness of the residents’ rooms, there are many impactful improvements to be made.
Selecting Furniture for Fall Prevention
When designing or remodeling your long-term care facility, your furniture selections can make all the difference in keeping residents safe. When designing common rooms, dining rooms, and resident rooms, choose chairs that have grip-able arm rests and a high seat-to-floor height. These features help residents ease themselves into a seated or standing position. Also, make sure that the upholstery is not too slippery and provides enough coefficient of friction to provide a stable seat. Some models of dining chairs also offer ball casters on the front legs to make it easier to scoot in or out from the table.
In resident rooms, plan a layout that allows the resident to access their personal belongings as safely and independently as possible. Rolling bedside tables are excellent solutions for placing personal effects within reach (i.e., remote controls, cell phones, books, medications).
Flooring for Fall Prevention
Floor surfaces have a massive impact on fall risk. Always make sure your custodial staff responds quickly to spills, thoroughly cleaning and drying the area. The carpeting should be low-pile and securely attached to the floor. While area rugs are typically discouraged in long-term care facilities, sometimes a resident will bring one from home. Make sure that the rug is equipped with a non-slip pad and has no wrinkles or curled edges that may pose a tripping hazard.
Cleanliness Counts!
It pays to keep hallways, common areas, and resident rooms free of clutter and debris that could cause a mishap. Common culprits include spills, dust, clothing left on the floor, and untidy cables and cords. During each visit to your residents’ rooms, always look for loose items on the floor and make sure there are no cleanliness issues to address.

How to Select Clothing that Reduces Fall Risk
While clothing is not typically a part of a treatment plan, small changes to a resident’s outfit and footwear can make a big difference for their safety. Here are some clothing items that should be avoided for residents in long-term care.
- Loose or Baggy Clothing – Loose articles can cause trip hazards or get caught on doorknobs, medical equipment, handrails, etc.
- Silky Pants – While comfortable, these make the seating surface unnecessarily slippery and can lead to sacral sitting and other unstable postures.
- Smooth-Soled Shoes – These footwear options don’t provide much traction, especially on smooth flooring surfaces like hallways.
- Slipper Socks – Socks can easily slip off the foot, and don’t support the foot or ankle.
- Thick-Soled Shoes – Soft cushioning can add comfort but also reduces stability in the gait.
Make Sure Personal Needs are Met to Reduce Falls
Residents with pressing physical needs will feel the urge to stand and find relief. This is why it’s critical for nursing staff to be attentive to needs like using the restroom, getting a drink, repositioning in bed, or finding pain relief. If these needs are unmet, residents may feel they are left with no choice but to try to help themselves, risking injury in the process.
Upon entering your resident’s room, make sure that you ask:
- Are you having any pain? If so, offer pain medication or schedule some for upcoming rounds.
- Are you comfortable with your position? If not, move them up in bed, offer them another pillow, bring a blanket, or anything else they may need to feel comfortable.
- Do you need to use the restroom? Assist them to the bathroom if they need help.
- Can I hand you anything? Do you need your phone, the remote control, a drink, your call light, or anything else you have dropped or might need on-hand until your next visit?
How to Choose a Wheelchair that Reduces Fall Risk
The goal of a wheelchair seating system is not only to provide comfort to the user, but also to help the user achieve a stable, healthy posture. Choosing the wrong wheelchair, however, can wreak havoc on a patient’s stability while seated. Wheelchair users demonstrating abnormal postures, such as a posterior pelvic tilt, have an even higher fall risk, and should take special care when selecting a seating system.
When selecting a wheelchair to reduce fall risk, be sure to consider sizing. If the wheelchair is too big, the person may be more likely to slide out of the wheelchair. If the seat width is too narrow, the wheelchair will create a squeezing effect, creating discomfort and increasing the likelihood the user will try to stand up unassisted. If the seat depth is too shallow, the femurs will not have adequate support which could cause a fall if the user leans too far forward. These are just a few examples of how wheelchair fit can increase the risk of an injury from a fall.
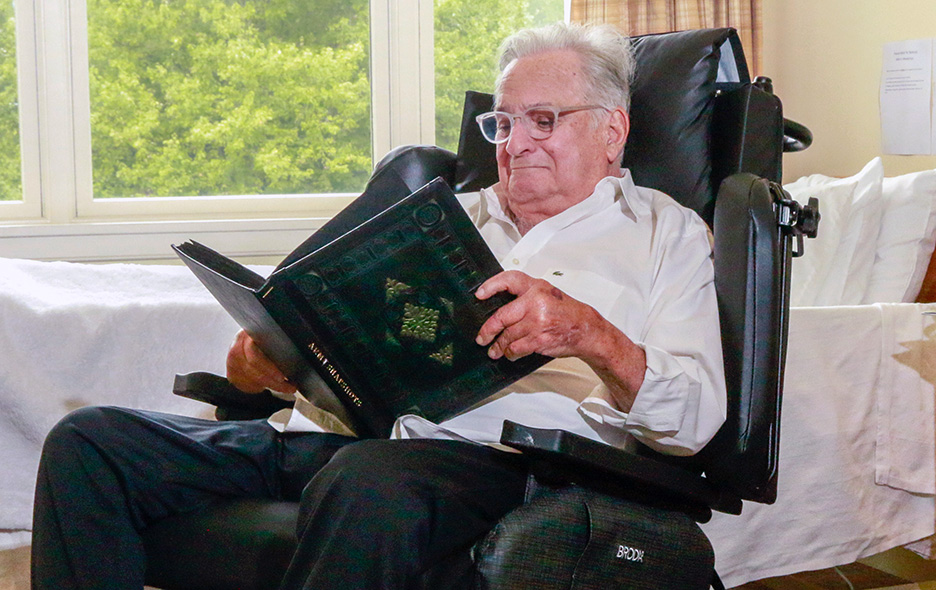
Broda wheelchairs are ideal for fall prevention programs in long-term care.
How to Correct an Unsafe Seating Posture
If you have a patient who is sitting in an unsafe posture, you need to consider the full picture. What is causing the person to sit this way? Are they in a standard sling-back wheelchair? Are their hamstrings tight? Most people’s bodies cannot accommodate sitting in the textbook posture of 90° x 90° x 90°. Many clinicians find that forcing this posture is like trying to fit a square peg into a round hole.
Rather than treating the symptoms, identify the cause of the abnormal posture, which is the key to preventing falls from the wheelchair.
Here are some common reasons for sacral sitting and sliding.
- Pressure injuries or other wounds
- Muscle tone issues
- Discomfort or pain
- Improper seating surfaces, such as a sling-seat wheelchair
Common Pitfalls to Avoid When Preventing Falls
While augmenting your fall prevention program, check that your nursing staff isn’t engaging in any of these harmful practices.
- Never elevate the lower leg supports in order to prevent falls. The elevation puts tremendous stress on the hamstrings and is known to cause additional pain.
- Avoid the use of pommel cushions. These put unnecessary pressure on the groin, and can cause pressure injuries in sensitive areas.
- Never place non-slip matting directly on top of the cushion. Non-slip materials, such as Dycem®, are only for use under a cushion. Placing it on top of the cushion can cause shear, which results in instant, invisible skin damage. Cushion covers generally have a high coefficient of friction to assist in keeping someone in their seat. Dycem has a very high coefficient of friction. With Dycem, instead of sliding on the cushion, the pelvis is sliding under the skin causing shear.
- Avoid using the “dump” maneuver, which elevates the front of the chair by raising the front caster wheels. While “dumping” can decrease sliding, it will also create pressure over the ischial tuberosities (ITs). Patients will then experience pressure injury on the ITs instead of the sacrum. “Dumping” also creates shear risk. Instead, the resident should use a tilt-in-space positioning wheelchair.
- Don’t forget that many patients with cognitive impairments will try to relieve pain and discomfort by attempting to stand, possibly placing them at risk for a fall. Take special care for residents with cognitive challenges like Alzheimer’s and other dementias.
Remember, any highly effective intervention must be consistently followed outside of therapy. Make sure that the entire care team is on board with the intervention plan. To accomplish this goal, communicate the plan clearly with verbal and written instructions, and have leadership check compliance regularly.

Implementing Changes at the Facility Level
While these fall prevention tips may seem simple for one individual, they’ll take a concerted effort to implement at the facility level. Facility Administrators should consult with their nursing team leadership to determine the procedure modifications, staff expectations, and monitoring practices to make sure the fall prevention program is as effective as possible. Small changes can make a big difference! Try focusing on just one area to start, and gradually increase the impact over time.
Recommended Wheelchairs for Fall Prevention
One overarching solution that can make a big impact is choosing the right wheelchairs for your residents at risk for falls. Broda wheelchairs have a proven track record of 40+ years of excellent fall prevention. Here are some of the top wheelchairs recommended by long-term care facilities across the country. All of these wheelchairs come equipped with Broda’s signature Comfort Tension Seating® system, which is clinically proven to reduce pressure better than a sling-seat wheelchair or basic foam cushion.
Synthesis Positioning Wheelchair
Who Should Use the Synthesis?
For caregiver-dependent residents, the Synthesis Positioning Wheelchair stands out as the gold standard of fall prevention.
Benefits of the Synthesis:
- Customized Positioning with Up to 40º of Tilt and 90º of Recline
- No-Lift Lateral Transfers
- Adjustable & Fully Removable Arm Rests & Shoulder Bolsters
- Supports Proper Posture Without Restraints
Encore Pedal Wheelchair
Who Should Use the Encore?
The Encore Pedal is best for residents who are independent and able to self-propel.
Benefits of the Encore Pedal:
- Low Seat-to-Floor Height (As Low as 12.5″)
- Excellent Proprioceptive Input
- Hand, Foot, or Hemi-Propulsion
- Customized Seat Tilt Up to 40º
- Optional Dynamic Rocking for Soothing Motion
- Bariatric Sizes Available!
Revive Shower Commode
Who Should Use the Revive?
The Revive Shower Commode is ideal for individuals at risk for falls and pressure injuries who desire a dignified, safe, and thorough bathing experience.
Benefits of the Revive:
- No-Lift Lateral Transfers
- Easy Skin Assessments
- Customized Positioning with 12º of Posterior Tilt, 10º of Anterior Tilt, and 67º of Recline
- Removable Arm Supports
- Fits over Standard Toilets
- Bariatric Sizes Available!
Please Note: The information provided in this blog post is intended for general informational purposes only and should not be considered professional medical or safety advice. Each healthcare facility and resident is unique and fall prevention strategies should be tailored to individual needs and environments. Always consult with qualified healthcare professionals and follow your facility’s protocols and regulations to ensure the safety and well-being of all residents.
Frequently Asked Questions
What is the definition of a fall?
The World Health Organization (WHO) defines a fall as: “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.”2
An accurate definition of falls includes any uncontrolled descents onto any surface. How about a forceful drop onto a bed or into a wheelchair? This could be a precursor to a fall and could also cause injury. Caution is always advised when performing transfers and when assisting individuals with balance impairments and muscle weakness.
What is the best wheelchair for fall prevention?
The best wheelchair to prevent falls will be the equipment that helps your patient achieve the most comfortable and aligned posture. The best fall prevention wheelchairs also have a stable seat surface and fit the individual correctly. Broda offers excellent manual wheelchairs for fall prevention that make everyday sitting more comfortable and transfers easier.
References
- Haskins, J. (2018). Falls among US seniors cost $50 billion each year. The Nation’s Health, 48 (4) E18. Retrieved from: https://www.thenationshealth.org/content/48/4/E18
- World Health Organization. (2021, April 26). Falls. Fact Sheets. Retrieved from https://www.who.int/news-room/fact-sheets/detail/falls
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS) [online]. Accessed March 11, 2024.
- Centers for Disease Control and Prevention (2021). Surveillance Report of Traumatic Brain Injury-related Hospitalizations and Deaths by Age Group, Sex, and Mechanism of Injury—United States, 2016 and 2017. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services.










